Converting blood types A, B into blood type O: Why does this breakthrough deserve the Nobel Prize in Medicine?
Nearly 100 years ago, Landsteiner won the Nobel Prize in Medicine after dividing human blood into four groups. Now, if someone could combine them all into one, that person would also deserve a Nobel Prize in Medicine.

Two seconds is the time it took you to read the title of this article. And somewhere out there, someone needs a blood transfusion. Traffic accidents, surgery patients, children with congenital anemia, cancer patients or even patients with hemorrhoids… they all need blood to survive.
The World Health Organization (WHO) says that each year, the world's need for blood is more than 150 million liters, equivalent to 304 million units. Unfortunately, with the current rate of blood donation, we can only meet about 90% of the need for blood transfusion.
And that's the number in developed countries.

In low- or middle-income countries, only about 50% of blood needs are met. Things are even more complicated when taking into account the matrix of 45 different blood types, and not everyone has the right blood type to donate and transfuse to people in need.
As a result, millions of people die each year because they have rare blood types or cannot receive timely transfusions. But from now on, these deaths could soon be a thing of the past.
In a new study published in the journal Nature Microbiology, a team of scientists from Denmark and Sweden have found an effective method to turn any blood type into type O blood, the compatible blood type. with all remaining blood types and can be transfused to anyone.
This would essentially equalize the matrix of 45 blood types that exist in the human body – a breakthrough that could save millions of lives worldwide and, if proven effective and feasible, would be worthy of a Nobel Prize in Medicine nomination.
Blood Transfusion: A Risky Procedure
The history of blood transfusions probably dates back to 400 BC when Hippocrates, the father of modern medicine, formulated the humoral theory. He proposed that the human body was a balance of four humors—blood, phlegm, black bile, and yellow bile.
When any fluid is deficient or excessive, it leads to an imbalance of the remaining fluids and causes disease. The cure is therefore sometimes just a matter of removing the excess of another fluid, and adding one when it is deficient.
For example, ancient medical texts record Hippocrates' idea of cutting into a patient's skin to drain blood, in cases where he thought their illness stemmed from excess blood.
On the contrary, with diseases originating from anemia, Hippocrates will "transmit" them back to the patient's body. But he did so in a very simple way: giving the patient healthy human blood to drink.
This idea not only existed in ancient Greek civilization, in Egypt and China, when a patient was considered anemic, doctors also simply thought that they could drink human blood or animal blood to regain health.
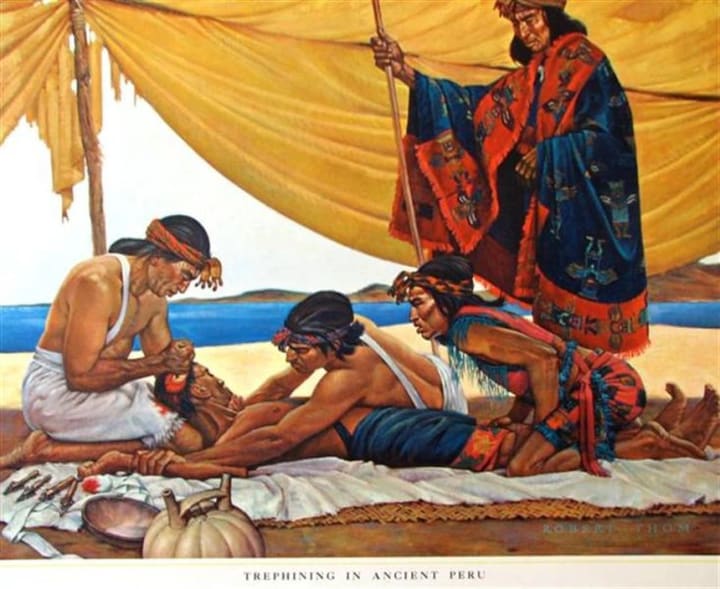
The first human-to-human blood transfusion turned out to be a product of South American civilization, during the Inca era. Records from Spanish conquistadors during their conquest of the Inca empire show that natives there used to give blood to each other during open-cranial surgeries.
The details of the procedure are not clearly recorded, but historians believe that the Incas actually gave blood to each other and had a very high success rate, because most South American natives had type O blood. Compatible with all remaining blood types.
Indeed, over the next 400 years, when doctors in the West tried to imitate the Incas for blood transfusions, their failure rate was significantly higher. In 1492, after Pope Innocent VIII of the Vatican fell ill and fell into a coma, his blood vessels were extracted and connected to the blood vessels of three 10-year-old boys.
As a result, all four people died.
By 1818, a British obstetrician named James Blundell had performed 10 blood transfusions on women suffering from postpartum hemorrhage. As a result, he saved the lives of five women, five of whom later died.
Throughout the 19th century, many blood transfusion attempts were made in Western countries, but the success rate was so close to chance that doctors were rarely interested in the idea.
Things only changed after Karl Landsteiner, an Austrian-American doctor, discovered the reason why blood transfusions fail. It was because the recipient and the donor had different blood types.

OAB
It was in 1901, while doing some experiments with blood collected from different members of his laboratory, that Landsteiner noticed that when he separated one person's serum from their blood, the serum could coagulate red blood cells isolated from another person.
This phenomenon is called hemagglutination, which Landsteiner speculates is a lethal reaction that occurs when blood is transfused between incompatible individuals.
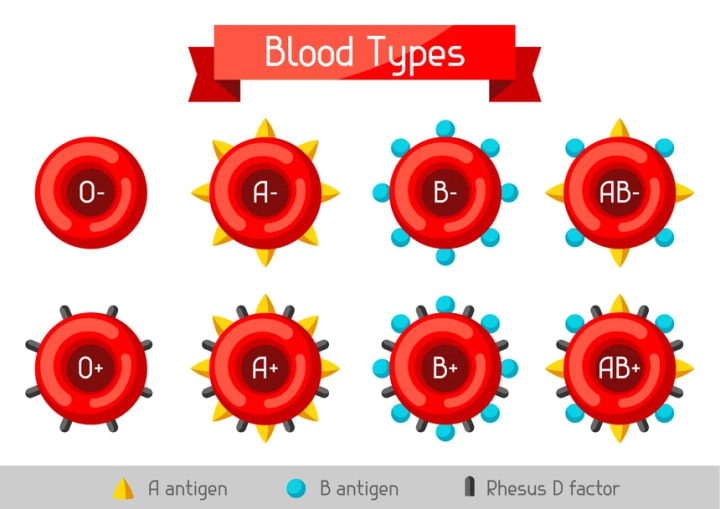
Through continuous experiments for a year, Landsteiner eventually identified two different types of antigens and antibodies in the blood, which he called A and B antigens and antibodies.
People who have A antigen on the surface of red blood cells will have B antibody in their serum. Landsteiner calls these people people with type A blood.
Conversely, people who have B antigens on the surface of their red blood cells will have A antibodies in their serum. They are called people with blood group B.
If there are no antigens on the surface of red blood cells but both A and B antibodies are present in the serum, Landsteiner called this blood group C (C was later renamed O from the German word for "Ohne", or "without", meaning no antigens on red blood cells).
In cases where red blood cells have both A and B antigens but the serum has no antibodies, this blood group is called AB.
Landsteiner found that agglutination occurs when antigens from one blood type pair with antibodies of the same type from the other blood type. Therefore, in principle, a person cannot receive blood with foreign antigens into the body.
For example, a person with blood type A cannot receive blood type B, because blood type B has B antigens that will pair with the B antibodies of blood type A and vice versa.
People with blood type O can donate blood to anyone, because their blood does not have antigens to agglutinate when encountering antibodies A and B in the other three blood types.
On the contrary, people with blood type AB can only transfuse blood to people with the same blood type AB because they have both antigens on the surface of red blood cells.
After Landsteiner discovered these blood types, he helped the rate of accurate blood transfusion increase, opening an era of safe blood transfusion. In 1930, Landsteiner was awarded the Nobel Prize in Medicine for his discovery of blood types. But things don't stop there.
+ and -
Ten years after receiving the Nobel Prize in Medicine, Landsteiner made another groundbreaking discovery. Together with his American colleague Alexander Wiener, he discovered another antigen called Rh – named after the rhesus monkey because this antigen is commonly found in monkey blood.
Rh is actually a system of more than 50 antigens, but the most important of them is the D antigen - the antigen that reacts most strongly with condensation.
People with Rh D antigens next to A and B antigens in red blood cells will be called blood types A+, B+, AB+ or O+. On the contrary, people who do not have it will have blood types A-, B-, AB- and O-.
Based on Landsteiner's principle, again, a person with the Rh D antigen in their blood cannot donate blood to a person without it. For example, blood type A+ cannot be donated to a person with blood type A-, and a person with blood type O+ cannot be donated to all blood types A-, B-, AB-, and even O-.
Only people with O- blood are truly compatible with all other blood types. Therefore, they are often referred to as potential blood donors.
People with blood type O- are often encouraged to donate blood and their blood will be reserved in large quantities to prepare for cases requiring emergency blood transfusions when doctors do not have time to wait for blood tests for patients, for example when someone is in a traffic accident.
Unfortunately, only about 6% of the world's population has O- blood, making the supply of this blood type very limited.
Scientists have long wanted to create an artificial type O- blood, by removing all the antigens from the red blood cells of other blood types. Until recently, though, they have failed.
The first notable attempt was made in 1982, when a group of researchers found an enzyme in coffee beans that could remove the B antigen and turn type B blood into type O blood. Unfortunately, it only worked under strictly controlled conditions and proved ineffective.
In 2017, another group of scientists was also able to create type O blood by inserting cancer-causing genes into red blood cell precursors. However, it seems that this idea is not safe at all, and the cost of this technique is also very large.
In 2019, in a work published in the journal Nature, scientists from the University of British Columbia presented a method of exploiting the DNA of bacteria in the human intestine, which can convert type A blood into type O blood. .
However, subsequent trials have not yet reached the safety level needed to commercialize this artificial O blood. For some mysterious reason, many patients are still incompatible with O blood even though their antigens have been removed.
There are over 45 blood types and we need to convert them all to O blood type
In a new study published in the journal Nature Microbiology, a group of scientists from the Technical University of Denmark and Sweden's Lund University explains that blood transfusion incompatibility in the OAB and Rh +- systems is actually comes from the fact that humans do not only have 8 blood types.
The A, B and Rh D +- antigens on the surface of red blood cells are actually molecular segments protruding from the cell. While they may be the same type, the length and density of antigens also differentiate a blood molecule, allowing it to be classified into a different blood type.
Scientists say that if analyzed more closely, human blood can be divided into 45 groups, based on the extent of A and B antigens. The number is even increasing over time.
Therefore, some previous techniques to neutralize A and B antigens for blood group O did not achieve complete effectiveness, for some blood groups A and B with expanded antigens.
" Here, however, we report the discovery of an enzyme that is remarkably effective not only against A and B antigens but also against their extensions ," the scientists said in the new study.
Specifically, they used an enzyme found in the gut bacteria Akkermansia muciniphila to treat blood from donors belonging to groups A, B, and their extended subgroups.
Living in the human gut, Akkermansia muciniphila is a bacterium that feeds on intestinal mucus to survive. Evolution has provided it with enzymes that break down the mucus on the surface of the intestinal lining, which scientists have found to be chemically similar to antigens found on red blood cells.
So, in this study, they tested 24 enzymes that the Akkermansia muciniphila bacteria secrete to process hundreds of blood samples.
The enzymes were incubated with high concentrations of red blood cells, at room temperature, for 30 minutes to effectively deplete all four A and B antigen extensions. This produced type O blood that was compatible with more than 91% of people requiring blood transfusions.
Previously in 2022, scientists also used a similar enzyme to convert eight lungs of people with blood type A to blood type O by removing all A antigens from these lungs.
The work was done within four hours, with a 97% reduction of the A antigen. The three lungs were then immersed in serum to simulate a real transplant.
As a result, scientists did not find agglutination lesions in these spectra, showing that they had compatible blood types.
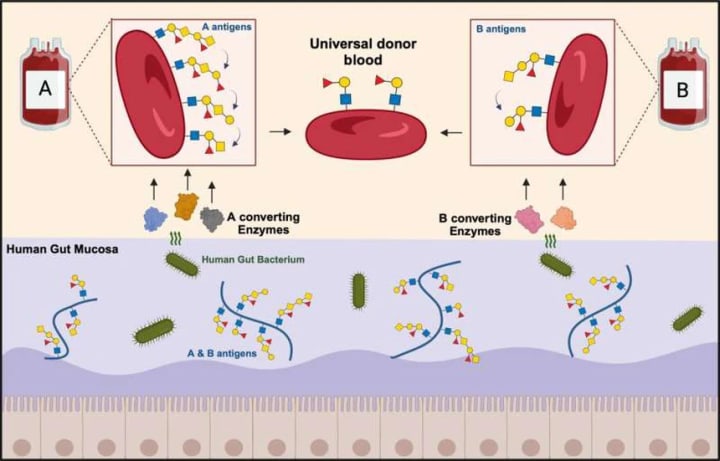
Now, with Swedish and Danish scientists finding an enzyme that removes all A and B antigens from the blood, they are moving toward the finish line, where all 45 ABO blood types can be neutralized. about blood type O-, compatible with all patients.
If this can be done, the world's need for blood supply will be solved.
In the near future, scientists will register a patent and conduct clinical trials with the blood type that reduces antigens with the Akkermansia muciniphila enzyme that they have created. If this test is successful, it will be a new turning point in the blood industry, where Landsteiner's 45 blood types will be brought together under one roof.
Nearly 100 years ago, Landsteiner won the Nobel Prize in Medicine for separating human blood into dozens of types. Now, if someone could combine them all into one, they would deserve a Nobel Prize, too. Because that discovery would save millions of lives, people who need a bag of O- blood every two seconds, right now.
About the Creator
HK Decor
Telling stories my heart needs to tell <3 life is a journey, not a competition
If you like what you read, feel free to leave a tip,I would love some feedback
https://sites.google.com/view/hk-decor/trang-ch%E1%BB%A7
Enjoyed the story? Support the Creator.
Subscribe for free to receive all their stories in your feed. You could also pledge your support or give them a one-off tip, letting them know you appreciate their work.






Comments
There are no comments for this story
Be the first to respond and start the conversation.